One Coronavirus Model Offers More Optimistic Projections
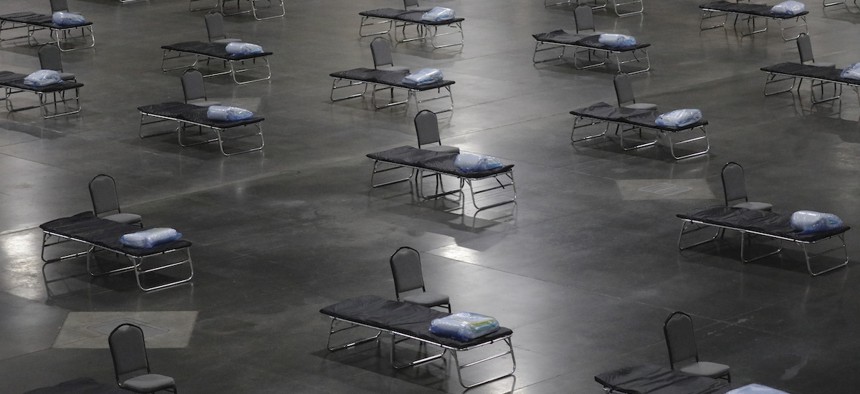
Beds are shown at the Mountain America Expo Center Monday, April 6, 2020, in Sandy, Utah. The state has contracted with Salt Lake County to use the facility as an alternate care site, or hospital overflow. Associated Press
An updated estimate from the University of Washington decreased the expected number of deaths related to Covid-19 by more than 11,000. But other models offer more devastating projections.
Health researchers working on one key model are predicting fewer deaths during the first wave of the coronavirus outbreak after receiving a “massive infusion of new data,” including state-level numbers of people hospitalized after contracting the disease.
The University of Washington’s Institute for Health Metrics and Evaluation forecasting model, which has been used by the White House, predicts that 81,766 people will die of Covid-19 in the United States through early August, according to an update released Sunday. The model's previous estimate, issued last Thursday, predicted 93,531 people would die from the highly contagious respiratory illness.
The updated model relies heavily on state-level data on hospital admissions. Previous updates were based on a CDC report on coronavirus cases nationwide from Feb. 12 to March 16, which totaled 509 hospital admissions and 46 deaths—a ratio of 11.1 admissions per 1 fatality. Using updated data from a handful of states, researchers calculated a new, much lower ratio, at 7.1 hospitalizations per death.
Those numbers are reflected in the lower death total, researchers said, but also in steep declines in the projections of hospital resources that will be needed during peak times. Sunday’s update predicts that at the height of the outbreak, hospitals will need a total of 140,823 beds (down from 262,092) and 29,210 ICU beds (down from 39,727), along with 18,992 ventilators (down from 31,782).
“These lower ratios of admissions to deaths result in predicted peak hospital resource use—total beds, ICU beds, and invasive ventilators—that is lower than previously estimated,” researchers said in an explanation of the update.
The data includes predictions for each state and the District of Columbia, including peak days (the date on which a state can expect to find its medical resources in greatest demand), deaths, and shortages of hospital beds, ICU beds and ventilators.
But other models are not offering these more optimistic scenarios. In Washington, D.C., Mayor Muriel Bowser on Friday said the model the city is using estimates that more than 90,000 people will be infected and the peak will come during the summer, the Washington Post reported.
“This is a tough number to have to report. But we think that we’d rather be on the side of underestimating the impacts of social distancing than presenting too rosy a picture," Bowser said. She emphasized there was still a need for more intensive care hospital beds and ventilators in D.C. to handle the cases they expect to see.
The Institute for Health Metrics and Evaluation model suggested that D.C. that same day had reached its peak number of cases and wouldn't need more hospital beds. It projected between 35 to 101 deaths in D.C. by early August, while the model the city is using from Penn Medicine estimates 220 people could die in a mild scenario to more than 1,000 in a severe one, the Post reported.
As of Sunday, the District of Columbia was reporting 1,097 Covid-19 cases, including 24 people who died from the illness.
IHME researchers made their projections in part on data from seven European cities where daily deaths have peaked after the implementation of social-distancing requirements that have largely kept people in their homes.
The model's state-level predictions assume that similar guidelines are in place, are strictly adhered to, and will remain in place all the way through May. Deviation from those circumstances dramatically alters the projections, said Dr. Christopher Murray, director of the institute.
"As we noted previously, the trajectory of the pandemic will change—and dramatically for the worse —if people ease up on social distancing or relax with other precautions,” he said in a statement. “Our projections are strengthened by the new downturns in more regions. This is evidence that social distancing is crucial.”
Still, some have noted the updated projections currently do not match the local reality. In Louisiana, for example, the model estimated that the height of medical resource demand peaked on April 1, and that deaths would peak on Friday and then drop consistently. But deaths because of the coronavirus rose “on three of the last four days,” wrote Jeff Adelson, a staff writer at the Times-Picayune/Advocate in New Orleans, on Monday. “That includes Sunday when 68 deaths were recorded, the highest number of deaths the state has seen on a single day.”
The model accounts for some variation—it predicted 42 deaths in Louisiana on Sunday, for example, but included a possible range of 15 to 88 deaths. But some of the discrepancies defy the ranges as well, Adelson wrote.
“According to the newer version of the model, Louisiana should have expected to have between 182 and 367 patients on ventilators on Sunday and between 751 and 1,620 patients in hospital beds,” he said. “In fact, the state reported 561 patients on ventilators and 1,803 patients in hospital beds on Sunday.”
In explaining the update, researchers noted that state-level information was used only from places that had reported data from 50 or more deaths related to Covid-19—a total of seven states (New York, Massachusetts, Georgia, Colorado, Pennsylvania, Florida and California). For states without that data, researchers based their estimates on the average of 7.1 hospitalizations per death, calculated using the information from those seven states. As more states compile specific data, the model will adjust, Murray said.
“As we obtain more data and more precise data, the forecasts we at IHME created have become more accurate," he said. "And these projections are vital to health planners, policymakers, and anyone else associated with caring for those affected by and infected with the coronavirus."
In addition to relying on broad social-distancing guidelines, the model assumes that states without strict protocols will issue them “within seven days,” Murray said.
"If social distancing measures are relaxed or not implemented, the U.S. will see greater death tolls, the death peak will be later, the burden on hospitals will be much greater, and the economic costs will continue to grow,” he said.
NEXT STORY: Census undercounts are normal, but demographers worry this year could be worse





