The Coronavirus Response is Straining an Already Depleted Public Health System
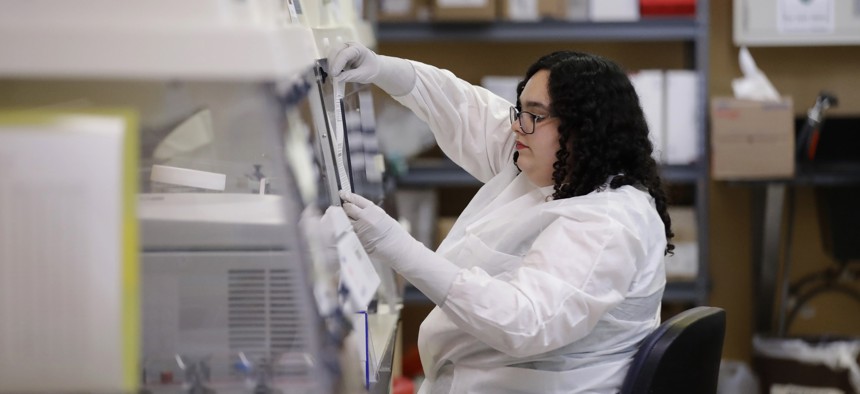
Aubrey Holland performs tests at the Bureau of Public Health Laboratories on Monday, March 2, 2020, in Miami, where the COVID-19 virus is being tested. Brynn Anderson/Associated Press
Years of funding shortfalls have left local health departments understaffed, vacancies that become particularly glaring during a large-scale emergency, advocates say.
Across the country, even in places where no patients have been diagnosed with the coronavirus, public health departments are mobilizing to respond to the outbreak. They do so after years of funding shortages and personnel cuts, shortfalls that advocates have long warned could interfere with the country’s ability to adequately respond to a widespread public health emergency.
“It’s certainly not ideal,” said Adriane Casalotti, chief of government and public affairs for the National Association of County and City Health Officials. “We need money for the activation of addressing coronavirus, certainly, but we also need to really be focused on what we are doing to support public health infrastructure writ large, year after year, so you aren’t starting from a place of deficit when you need to mobilize.”
The outbreak of novel coronavirus, a new strain of an existing respiratory ailment, has killed nearly 3,000 people in China and sickened tens of thousands of others. As of Wednesday, there were more than 100 confirmed cases in the United States. At least nine people have died and there are diagnosed patients in 12 states, including at least 27 patients in Washington and six in New York. The World Health Organization estimated the global death rate from the virus at around 3.4%, but the overall risk to the general public remains low in the United States, according to the Centers for Disease Control and Prevention.
The emergence of the virus comes after years of budget cuts to public health, a trend that began during the Great Recession and never really stopped. Public health programs received $675 million in funding in the most recent fiscal year, down from $900 million in 2005. Budget cuts led to the elimination of more than 55,000 local health department positions from 2008 to 2017, according to the nonprofit Trust for America's Health.
Those shortages become particularly noticeable after a year of continuous public health issues—outbreaks of measles and hepatitis A, a mysterious vaping-related illness, prolonged debates about the effectiveness of vaccines, historically high levels of sexually transmitted infections—followed, now, by an outbreak of a new illness, Casalotti said.
“If you work in public health, you know there’s always a new issue, but nationally it really feels like the public health issues are coming in more severely and more frequently,” she said. “During all of these things, you’re not just pulling from fewer staff, you’re asking the same staff to keep working at 130% over and over again, shifting from issue to issue as each one becomes a priority.”
Some states have taken steps to authorize supplemental funding for public health efforts during the outbreak of COVID-19. Florida and Washington declared states of emergency. Lawmakers in New York approved $40 million for coronavirus preparations, while Maryland Gov. Larry Hogan announced $10 million in emergency funding and California Gov. Gavin Newsom asked lawmakers in his state for $20 million.
For their part, federal lawmakers began voting on more than $8 billion in federal aid on Wednesday, with a package passing the House. That money is desperately needed for mobilization efforts, Casalotti said, which aren’t funded through typical budgetary measures at the state or local level.
“The way that local health departments are funded is very programmatic and specific, so it’s not like there’s a reserve pot of money when something like this happens,” she said. “Dollars are cordoned off for different types of activity, and even preparedness dollars do not sit in a pot of money waiting there for you when you need to respond to something. Those dollars are there to build the system and keep the cobwebs off, so to speak, and now we’re in the activation stage, and there is no funding for that.”
The cost of managing the outbreak is unclear and varies from place to place. In King County, Washington, for example, health officials have estimated that containment work costs around $200,000 per week. Much of that work revolves around what's known as disease investigation, where health officials interview confirmed patients about their movements in the days before they became sick, reconstructing a map that helps identify other people who may have been exposed to the virus. The health department there is also setting up temporary quarantine villages, consisting of clusters of trailers where infected patients can receive access to isolated treatment.
In some cities, departments have worked to redirect existing grant funding toward containment efforts, or have pulled money from state or local general funds. In others, public health officials continue to do the work without knowing how they’ll pay for it.
“We’ve heard from jurisdictions that are saying, ‘We don’t know where the money is going to come from but we know what we need to do to act, so that’s what we’re going to do,’” Casalotti said. “Some big cities are better resourced, even if they’re not well resourced. But as the virus spreads across the country there are going to be more places that don’t even have the capacity to start on the response level at all and are making those decisions without knowing where the financing is going to come from.”
As state and federal officials debate the details of supplemental funding, public health advocates are hopeful that the conversation will include discussion of shoring up the infrastructure as a whole. Local officials will control response to the virus either way, Casalotti said, but without sustained changes in funding, that response will come at the expense of other public health priorities.
“They are prepared and they will find a way to make it work—it’s just at what cost,” she said. “That’s the part that’s not sustainable.”
Kate Elizabeth Queram is a Staff Correspondent for Route Fifty and is based in Washington, D.C.
NEXT STORY: Insurers Sank Connecticut’s ‘Public Option.’ Would A National Version Survive?





