In Tackling Opioid Epidemic, Bold State Actions Needed for Data Analysis Efforts

Connecting state and local government leaders
Prescription drug monitoring programs aren't enough.
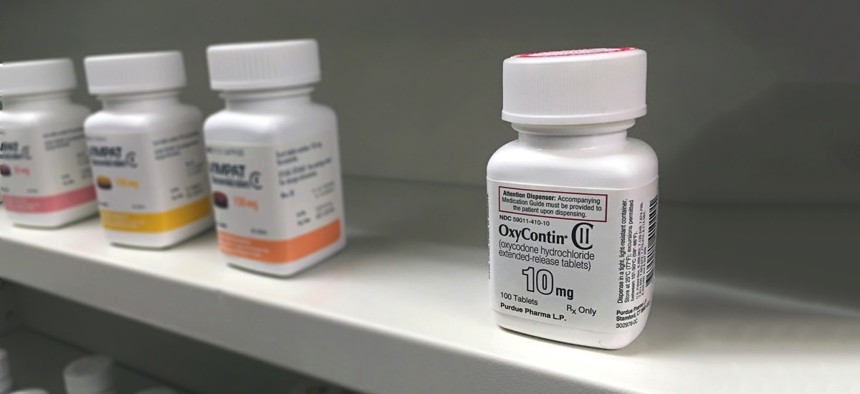
Opioid abuse, misuse and overdose deaths plague the United States, and countries worldwide. Most states have seen increases in opioid-related deaths, despite the use of Prescription Drug Monitoring Programs to significantly reduce opioid prescriptions.
PDMPs should be lauded for integrating data on prescribers, patients and dispensers. But, additional data needs to be analyzed to fully understand the opioid epidemic. Quite often, the required data is kept out of reach due to state statutes. Thoughtful and deliberate legislation can allow for the data to be used to create deeper understanding of the opioid problem, and better policies. It’s never been more critical than now.
To confront the opioid crisis, Congress passed the Comprehensive Opioid Abuse Reduction Act of 2016. Unfortunately, the Act fails to provide ample funding for substance abuse programs, which are a crucial part of breaking the cycle of addiction.
Without treatment plan availability or recovery services, those struggling with addiction are driven to a marketplace where an abundance of illicit drugs are available at a fraction of the cost of their pharmaceutical equivalents. Further, these illicit drugs are often combined with other dangerous substances, with varying efficacy. These combinations often overwhelm the addict, which can lead to unintentional death. To develop a comprehensive strategic plan to thwart the ongoing abuse and loss of life states need to take a look at the problem from a holistic level.
This is the path the Commonwealth of Massachusetts embarked on, but it took bold action from the legislature. Commonwealth policies makers passed legislation to allow the MA Department of Public Health to create a new data model to analyze ten data sets across seven agencies, while safeguarding privacy and complying with policy concerns.
Preliminary findings in the first report from the Massachusetts Department of Public Health were troubling, but not surprising. For instance, the research confirmed suspicions about the risks associated with mixing medications, and “doctor shopping.” Doctor shopping is when a person attempts to obtain opioid prescriptions from multiple medical professionals over short periods of time. This behavior increases the potential for addiction and overdose.
The report indicates “the concurrent use of benzodiazepines and opioids is associated with a 4-fold increase in risk of fatal opioid overdose.” Also, the use of 3 or more prescribers within a 3 month period is associated with a 7-fold increase in risk of fatal opioid overdose”.
Additionally, the report uncovered data gaps when attempting to identify nonfatal opioid-related overdoses. It states, “…at least 30 percent of Massachusetts Ambulance Trip Record Information System data was unreported and only 20 percent of data from MATRIS and Case Mix (hospital data collected on patient demographics, diagnoses and procedures, physicians, and charges for each inpatient discharge, outpatient observation stay, and emergency department visit) overlap…”
The implication of the missing data is that Massachusetts could be significantly undercounting non-fatal overdoses. It’s critical for states to identify gaps like this to improve overall data quality and produce more accurate analyses.
These are insights that can only be gleaned by disparate agencies collaborating to integrate multiple data sources. Having spoken to many state officials regarding this very topic, I know it is one of their most frustrating challenges.
PDMPs should be recognized for great strides in aggregating opioid prescriptions for prescribers and dispensers. Doctors and pharmacies are better informed when prescribing these highly addictive substances, highlighting individuals who may be doctor shopping.’ PDMP data helps the medical community and regulators safeguard patients more effectively through transparency of controlled substances across medical specialties. It reduces doctor shopping, dissuades abuse and misuse, and promotes responsible prescribing practices.
However, PDMP data alone only provides insight into a small portion of the opioid challenge. Many states struggle with varying issues in bringing together additional, multiple data sources to address the opioid epidemic. Emergency room visits, substance abuse treatment programs, criminal justice data, and mortality reports, just to name a few, are critical in understanding the true scope of the challenge. We need more insight into the leading and lagging indicators of unintentional overdose deaths, high risk indicators and other information that can help our leaders make effective decisions on legislation, funding, and programs aimed at driving change in this area.
The Commonwealth of Massachusetts is leading the way in establishing data models that satisfy all parties concerned, which is one of the most challenging obstacles to overcome. This type of innovation will help other states quickly overcome similar barriers to speed the time to insight, saving more lives in the process.
A former intelligence analyst in the U.S. Army, Jen Dunham now serves in the SAS Security Intelligence Global Practice. Dunham provides expertise on various security risks such as cyber security, insider threats and other Intelligence-specific applications of SAS Analytics.

NEXT STORY: Tax Credits for Ramps, Grab Bars to Help Seniors Stay at Home




