Rural Hospitals in Greater Jeopardy in Non-Medicaid Expansion States
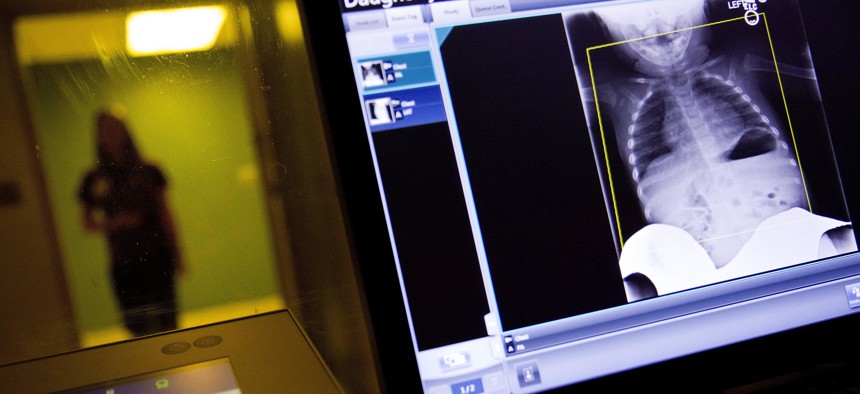
A radiology technician looks at a chest X-ray of a child suffering from flu symptoms at Upson Regional Medical Center, a rural hospital in Thomaston, Ga., on Feb. 9, 2018. AP Photo
Of the 600-plus rural hospitals at risk of closing, Texas has the most facilities in danger, a study found.
This story was originally published by Stateline, an initiative of The Pew Charitable Trusts.
In crime novelist Agatha Christie’s biggest hit, “And Then There Were None,” guests at an island mansion die suspicious deaths one after another.
So you can forgive Jeff Lyle, a big fan of Christie’s, for comparing the 36-bed community hospital he runs in Marlin, Texas, to one of those unfortunate guests. In December, two nearby hospitals, one almost 40 miles away, the other 60 miles away, closed their doors for good.
The closings were the latest in a trend that has seen 21 rural hospitals across Texas shuttered in the past six years, leaving 160 still operating.
Lyle, who is CEO, can’t help wondering whether his Falls Community Hospital will be next.
“Most assuredly,” he replied when asked whether he could envision his central Texas hospital going under. “We’re not using our reserves yet, but I can see them from here.”
It’s not just Texas: Nearly a hundred rural hospitals in the United States have closed since 2010, according to the Center for Health Services Research at UNC Chapel Hill. Another 600-plus rural hospitals are at risk of closing, according to an oft-cited 2016 report by iVantage Health Analytics.
Texas had the most hospitals in danger of closing (75), the health metrics firm said. And Mississippi had the largest share of hospitals at risk (79 percent).
Neither state has expanded Medicaid eligibility to more of its low-income residents under the Affordable Care Act, also known as Obamacare. In fact, the closures and at-risk hospitals are heavily clustered in the 14 states that have not expanded.
Those state decisions not to expand have deprived rural hospitals, which already operate with the slimmest of margins, of resources that could be the difference between survival and closure.
That is why Lyle and administrators of other rural hospitals in Texas and other non-expansion states are so adamant about their states joining the ranks of those that have expanded.
“It would mean a fair number of people we see who have no insurance would have insurance,” Lyle said. “And for us, a dollar is better than no dollar.”

In Texas, expansion would make 1.2 million more people eligible for Medicaid, according to a 2018 Kaiser Family Foundation analysis. An Urban Institute study in 2014 estimated that not expanding Medicaid would deprive Texas hospitals of $34.3 billion in federal reimbursements over 10 years.
Without that money, many rural hospitals in Texas and other non-expansion states have closed obstetrics units and other expensive services, forcing patients to travel long distances to seek treatment at the next-closest hospital, which is sometimes hours away.
By shedding those services, the hospitals diminish their reason for existing, said Maggie Elehwany, head of government affairs and policy for the National Rural Health Association.
The office of Republican Texas Gov. Greg Abbott and the most recent Republican chairmen of the health committees in the Texas legislature (the legislature has yet to make committee assignments for the current legislative session), Sen. Charles Schwertner and Rep. Four Price, did not return calls requesting comment for this story.
But not everyone believes Medicaid expansion is the answer to the problems facing rural hospitals. “Medicaid is as likely to prop up inefficient and wasteful hospitals as anything else,” said Michael Cannon, director of health policy studies at the libertarian Cato Institute.
Another rural hospital in Texas, Goodall-Witcher in Clifton, which also operates two community health clinics and a nursing room, risked closing until residents of Bosque County voted in November to create a hospital taxing district.
“I’m not saying we would have closed the day after the election,” said Adam Willmann, the hospital’s CEO, “but I don’t know how much longer we could have gone.”
The additional taxes will bring the hospital an estimated $2.5 million a year and perhaps take it out of the red, but they won’t necessarily lift Goodall-Witcher out of financial peril, Willmann said.
“Medicaid expansion,” Willmann said. “That is one of the key things we could do to help us deal with the tough financial demands we face.”
Burden of Uncompensated Care
As envisioned by the ACA when it passed Congress in 2010, expansion states would extend benefits to all adults— including childless adults—whose income was at or below 138 percent of the federal poverty line. (In 2019, that would be an average individual income of $12,140, depending on the state.)
Initially, the federal government paid 100 percent of the health care costs of the expansion population. The federal share falls to 90 percent in 2020.
To date, 36 states plus Washington, D.C., have expanded Medicaid. By 2017, expansion under the ACA had covered 17 million new enrollees. Roughly another 4 million people would qualify in the remaining states, according to a 2018 Kaiser report.
Instead, many of those low-income residents remain uninsured or underinsured in plans with high deductibles and copayments.
But that doesn’t mean people don’t receive health care. Without health insurance, low-income people are less likely to get preventive care, which often results in worsening health conditions that frequently bring them to hospitals where they are guaranteed treatment. Under federal law, hospitals must stabilize and treat anyone showing up at the emergency room, regardless of their ability to pay.
Rural hospitals, like their urban counterparts, are forced to absorb those costs. But unlike bigger hospitals, their patient volumes and operating margins are so low that “uncompensated care” burdens can be crippling.
For instance, Willmann said his hospital’s uncompensated tab last year was about $4.2 million, or 11 to 12 percent of his overall budget.
According to the Oklahoma Hospital Association, the state’s rural hospitals carried about $170 million in bad debt from charitable care and patients’ unpaid bills. Five rural hospitals have closed in the state since 2016.
A 2018 study in the journal Health Affairs found that the rate of closures of rural hospitals increased significantly in non-expansion states after 2014, when states began implementing the expansion. At the same time, closure rates decreased in expansion states.
‘99 Other Wounds’
Many administrators of rural hospitals are quick to say that Medicaid expansion alone will not solve their financial problems. Rural hospitals faced steep challenges long before the ACA.
Rural Americans tend to be older, in poorer health and less insured than those living elsewhere, the latter resulting in a greater share of uncompensated care for rural hospitals. Because of declining populations in rural areas, hospitals there often have empty beds, which means less revenue.
“It’s been a long, slow bleed,” said Fred Blavin, a health policy expert at the Urban Institute.
Automatic federal budget cuts beginning in 2013 (known as sequestration) reduced Medicare reimbursements, which are a particularly important source of revenue for hospitals. Congress has cut back on the amount hospitals can deduct for bad debt. Congress, in its budget tightening, reduced other forms of assistance to rural hospitals as well.
“You can put a Band-Aid on, but you still have 99 other wounds,” Willmann said.
Elehwany, of the National Rural Health Association, said that rural communities where hospitals are forced to close might be able to meet residents’ health needs by opening a new urgent care facility or maternal care center.
The loss of rural hospitals not only means patients having to travel longer distances to the next medical providers, but the closures also can often have a crippling effect on the local economy.
Goodall-Witcher Hospital is the largest employer in Bosque County. “Our payroll is bigger than the county’s entire budget,” Willmann said. “Can you imagine what it would do to this county to lose $9 million from the economy a year?”
A Health Services Research journal report found that when a rural area’s only hospital closes, income per capita falls by 4 percent and unemployment rises by 1.6 percent.
Willmann was relieved voters in his district supported the measure to create a hospital taxing district, but he acknowledged that it wasn’t a good deal for his county’s taxpayers. Their federal taxes help pay for the expansion in other states but not in Texas.
“Basically, you’re asking them to pay twice,” he said.
Rural hospital officials appear not to have the slightest hope that the deep red Texas legislature and governor will get behind expansion.
“There is no likelihood of Medicaid expansion in Texas in the near term,” said John Henderson, CEO of the Texas Organization of Rural & Community Hospitals.





