How COVID-19 in jails and prisons threatens nearby communities
With the highest incarceration rate in the world, the United States is particularly vulnerable to diseases spreading near correctional institutions.
COVID-19 has raged throughout U.S. jails and prisons, where people live together in close quarters and there is little opportunity for social distancing, a lack of basic sanitary supplies and high rates of chronic disease.
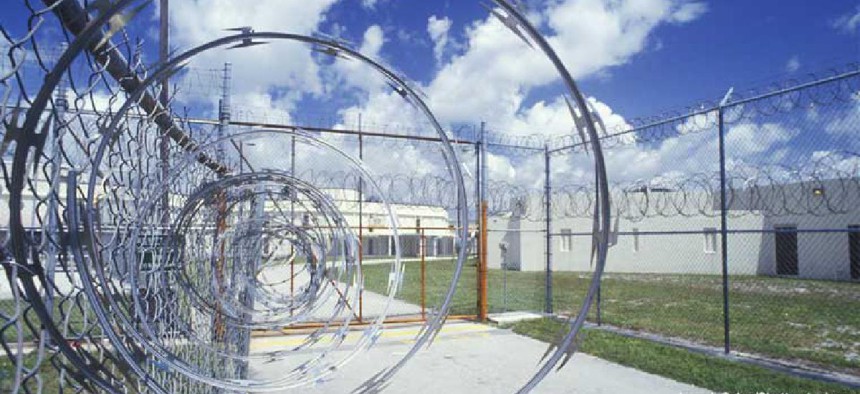
While inmates mostly stay behind concrete walls and barbed wire, those barriers can’t contain an infectious disease like COVID-19. Not only can the virus be brought into jails and prisons, but it also can leave those facilities and spread widely into surrounding communities and beyond.
The effect may be most pronounced in jails, which mainly house those who are awaiting trial or inmates serving short sentences. Those facilities tend to have more churn than state and federal penitentiaries, with greater numbers of people entering and leaving, thereby increasing opportunities for the disease to disseminate.
Two new studies show that jails can contribute enormously to coronavirus case totals outside their walls. While COVID-19’s spread inside the facilities has been widely reported, the research demonstrates just how great an impact it can have in communities outside.
Depending on the social distancing measures put in place, community spread from infections in jails could add between 99,000 and 188,000 people to the virus’ U.S. death toll, according to a modeling study recently published by the American Civil Liberties Union in conjunction with researchers from the University of Pennsylvania, the University of Tennessee and Washington State University.
The report was released in April, when some experts were predicting that the U.S. death toll would remain below 100,000. As of June 30, more than 125,800 people have died of COVID-19 in the United States.

A peer-reviewed study set to appear in the health policy journal Health Affairs echoes that finding. The researchers found that cycling through Cook County Jail was associated with 15.9% of COVID-19 cases in Chicago and 15.7% in Illinois as of late April.
“Although currently available data are inadequate to establish a clear causal relation,” the study’s authors write, “these provisional findings are consistent with the hypothesis that arrest and jailing practices are augmenting infection rates in highly policed neighborhoods.”
Cook County officials, including officials from the Chicago Department of Public Health, have pushed back hard on the report, calling it a “fantasy filled with assumptions bordering on lies.” They say it is based on old data that did not account for changes the jail had made to stop the spread of the virus, including testing and allowing for quarantining.
According to the county sheriff’s office, as of last week, 778 inmates at the county jail and 362 of its workers tested positive for the virus. Seven inmates and three employees have died.
The authors of the Health Affairs paper said they stand by their conclusions.
‘Correctional health is public health’
COVID-19 already has infected about 60,000 prisoners and correctional staff and killed more than 600 of them, according to the Marshall Project, which tracks the virus’ toll in correctional facilities. Many jails and prisons have reduced their inmate populations to reduce exposures.
The results of the ACLU and Health Affairs studies underline a point that many in public health have long advanced: Public health in the wider world is tethered to the health of those who are incarcerated.
“This is why public health officials say correctional health is public health,” said Dr. Brie Williams, a professor and researcher at the University of California San Francisco School of Medicine and director of Amend, a group that works to improve inmate health.
It’s not only released inmates, many of whom end up in crowded homeless shelters, who might carry the virus into communities. There are also risks of infection from inmates making court appearances or receiving medical care at hospitals in the community.
Infectious diseases move back and forth between communities and prisons. That was the case with tuberculosis in the 19th and 20th centuries and with HIV/AIDS in the 1980s and beyond.
In recent years, that point was made again in relation to hepatitis C, a communicable disease with high rates of infection in prisons because of the large numbers of incarcerated intravenous drug users. Sharing needles is one of the primary means of hepatitis C transmission.
One of the arguments public health experts used to urge local, state and federal governments to treat inmates with hepatitis C with highly effective but expensive medications was that knocking out the infection in prisons would prevent its spread beyond those walls. The difference between this pandemic and those other diseases, epidemiologists say, is that because COVID-19 is transmitted through respiratory droplets in the air, it spreads much more easily.
The other U.S. epidemic
The United States is particularly vulnerable to diseases spreading near correctional institutions. Its incarceration rate is the highest in the world, at 655 people out of every 100,000, according to World Prison Brief. With 2.1 million inmates, the United States also imprisons more people than any other country, nearly 412,000 more than China, which ranks second.
About 738,000 of those prisoners are in local jails, according to the federal Bureau of Justice Statistics. But that number is just a point-in-time snapshot. During the course of a year, 4.9 million people cycle through local jails, according to the Prison Policy Initiative, a Massachusetts think tank.
Additionally, federal labor statistics show that jails employ about 151,000 correctional officers who can bring infections into facilities or take them home.
Most cases in jails have not originated with inmates, said Dr. Alysse Wurcel, an infectious disease physician at Tufts Medical Center who sees patients at six area jails and is a consultant to the Massachusetts Sheriffs’ Association. “We’ve discussed with the sheriffs’ association that early on, clusters were initiated by people working in the jails, not by those newly incarcerated.”
There is a racial component to the concern about prisons and the pandemic. Disproportionate numbers of inmates are people of color, and the coronavirus is killing Black and Hispanic people at higher rates than their shares of the overall population. Those two data points have not escaped the notice of public health experts.
“We’re in an epidemic of mass incarceration of Black people at the same time as a disease epidemic that is disproportionately affecting minorities,” said Dr. Liz Barnert, an assistant professor of pediatrics at the UCLA David Geffen School of Medicine, who studies correctional health.
The pandemic has lent impetus to the growing movement to depopulate jails and prisons. Since the pandemic began, many states and local jurisdictions have taken steps to reduce inmate populations, releasing nonviolent offenders, granting more compassionate-releases and issuing citations rather than arresting alleged offenders.
Jails in California, Michigan, Massachusetts and North Dakota have released hundreds of prisoners. So have state prisons in those and other states. Many jurisdictions report large decreases in arrests.
Other states have done relatively little. Just last week, the Omaha World-Herald reported that the Nebraska prison system is 51% above capacity.
Public health experts insist that reducing jail and prison populations must continue, for the greater good of all.
“Decreasing the risk of spread of COVID-19 in jails and prisons decreases the risk of spread out in communities,” Williams said. “And increasing the spread in jails and prisons increases the risk of spread in communities.”
This article was first posted on Stateline, an initiative of The Pew Charitable Trusts.
NEXT STORY: Pandemic, China Trade Deal Fuel Farmer Doubts





