How States are Stifling Treatment for People Struggling With Opioids
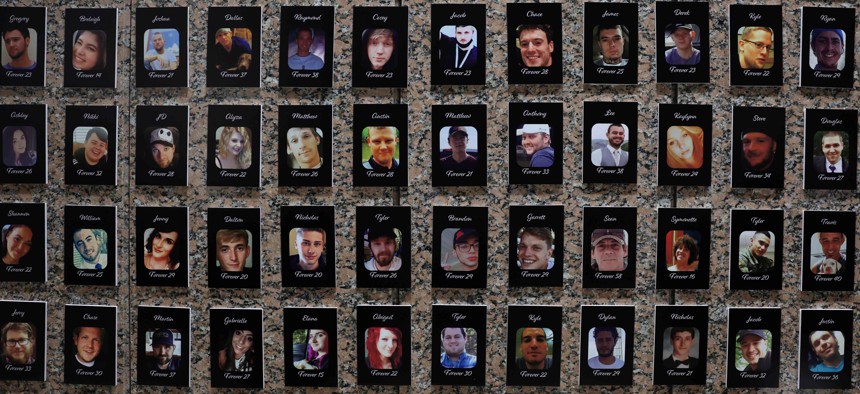
Photos of fentanyl victims are on display at The Faces of Fentanyl Memorial at the U.S. Drug Enforcement Administration headquarters on September 27, 2022 in Arlington, Virginia. Advocates say that nurse practitioners could help provide treatment to more people struggling with opioids. Alex Wong/Getty Images
COMMENTARY | Nearly 90% of people with opioid use disorder aren’t getting medical treatment. Nurse practitioners can help provide that care, but are limited from doing so in 24 states.
The deadly impact of opioids on our nation cannot be overstated. Nearly 75% of all U.S. drug overdose deaths in 2020 involved an opioid, and the epidemic is poised to enter a frightening new phase. A recent study from the Northwestern University Feinberg School of Medicine confirms that rural and urban counties could soon experience a significant increase in deaths from opioid overdoses as illicit fentanyl and other substances continue to flood into our communities.
Contributing to this crisis, nearly 90% of people living with opioid use disorder now aren’t receiving medication treatment – lifesaving medication treatments have shown to reduce the rates of overdose by roughly half. One answer to this national emergency lies in better access to treatment.
As a nurse practitioner in Oregon who is trained and authorized to prescribe medication-assisted treatment, I regularly treat patients with medications, such as buprenorphine and naltrexone. Methadone is a medication that can only be prescribed in outpatient treatment centers. These medications are a safer alternative to treating opioid use disorder and preventing overdoses. I know firsthand that it saves lives. I also know that in the 24 states without Oregon’s modernized policies, patients and communities are severely limited in their ability to access this lifesaving care.
At my health care clinic, I recently treated a patient with opioid use disorder and hepatitis C. I prescribed buprenorphine to reduce their cravings, and because I work in primary care, we also treated their hepatitis C with antivirals. This patient has now been in recovery for more than two years, was cured of hepatitis C, has been promoted to a higher-paying position at work and will be getting married at the end of the year. It’s critical that we provide the best health options for recovery to those living with opioid use disorder.
These medications work well, but many patients with opioid use disorder do not have adequate access to health care providers who can prescribe them. Access is not equitable across the country. While nurse practitioners prescribe this therapy, their ability to do so is stifled in some states. Nurse practitioners encounter state scope of practice laws that limit the services they can provide to patients, thus reducing their ability to provide valuable lifesaving care.
Oregon is among 26 states, the District of Columbia and two U.S. territories with Full Practice Authority, meaning that nurse practitioners can practice to the full extent of our education and clinical training and give patients direct access to the care we provide. The remaining 24 states have outdated regulations in place that restrict access to nurse practitioners, leaving patients without treatment, and in turn, without HIV and hepatitis C prevention.
According to data from the Substance Abuse and Mental Health Services Administration and the American Association of Nurse Practitioners, the states with the highest proportion of nurse practitioners with waivers to prescribe buprenorphine—Maine, Vermont, Alaska, New Hampshire and Oregon—all are states with Full Practice Authority, with 17%-21% of nurse practitioners holding waivers.
Conversely, the states with the lowest proportion of nurse practitioners with buprenorphine waivers– Tennessee, Alabama, Georgia, Mississippi and Texas—are states that reduce or restrict our practice authority, with less than 2.5% of nurse practitioners holding waivers. This inequitable access to treatment based on a patient’s geographic location means that some patients in our country who are struggling with substance use disorders have limited access to medication-assisted treatment.
We need all hands on deck including our nation’s 355,000 nurse practitioners to treat people living with opioid use disorder. States with reduced and restricted practice authority must modernize the outdated and restrictive laws that stand between patients, providers and the treatment patients need. These barriers have real consequences. They limit options for patients and their recovery, and in too many cases, they cost lives.
Laurel Hallock-Koppelman is a licensed nurse practitioner practicing in Oregon and a member of the American Association of Nurse Practitioners.
NEXT STORY: The Important Role Played by Secretaries of State in Administering Fair Elections is Changing





