Strengthening Medicaid should remain a national imperative
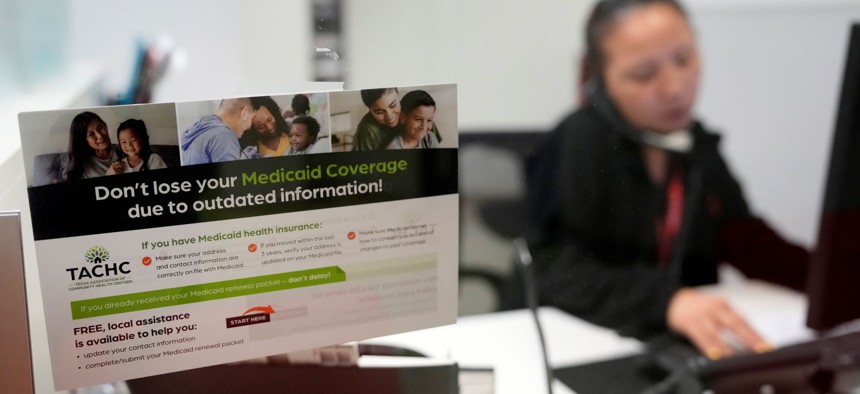
A reminder about Medicaid coverage is displayed as Trina Le, eligibility supervisor team lead, works at Hope Clinic, 7001 Corporate Dr., Tuesday, May 30, 2023, in Houston. Melissa Phillip/Houston Chronicle via Getty Images
COMMENTARY | Congress and state lawmakers should do everything in their power to ensure that anyone who needs Medicaid now and in the future is able to get it.
On Dec. 1, North Carolina became the 40th state to implement Medicaid expansion. For 600,000 residents newly eligible for one of the most effective health insurance programs in the United States, it was a life-changing day. Everyone in the country—regardless of who they are, where they live or how much money they make—should have health insurance. Strengthening Medicaid moves us closer to that goal and achieving health equity.
The largest health insurance program in the United States, Medicaid now provides free or low-cost coverage to more than 83 million people—but the program is at a crossroads. Thanks in large part to considerable Medicaid coverage gains in recent years, the national uninsured rate dropped to record-low levels in early 2023. But with states now disenrolling millions of people due to the end of continuous coverage protections, the number of individuals losing access to Medicaid is growing at an alarming rate. Congress and state lawmakers should do everything in their power to ensure that eligible people—especially children—do not lose coverage inappropriately and that anyone ineligible for Medicaid can quickly secure alternate paths to coverage.
Created in 1965, Medicaid is jointly funded by federal and state governments, with states administering their own programs. Specific eligibility differs by state, but participants—most with little or no income—generally include children, seniors, pregnant women and people with disabilities. Serving approximately one in four Americans, Medicaid is crucial to the nation’s health.
Few periods in Medicaid’s nearly 60-year history have been as consequential as the past decade. Jan. 1 marks the 10-year anniversary of states being permitted to expand their Medicaid programs under the Affordable Care Act, or ACA, with federal funds covering the vast majority of the expansion costs. Expansion has not only led to higher health insurance participation overall, but also a narrowing of racial and ethnic disparities in coverage and care—a distinctive achievement in a country where skin color and income level still disproportionately affect health outcomes. The results: better health outcomes—including tens of thousands of lives saved between 2014-17—lower health care costs, reduced medical debt for participants, along with more revenue and budget savings for states.
Medicaid also played a critical role during the COVID-19 pandemic. Under the Public Health Emergency, states were required to maintain continuous coverage for Medicaid participants and received additional federal funding for program administration. As a result, more than 22 million additional people received Medicaid coverage between February 2020 and March 2023. Since 2022, all but 4 states—including some that have not expanded Medicaid writ large—have extended Medicaid postpartum coverage from two months to a year, a critical step toward reducing America’s unconscionably high maternal mortality rate. All states will soon be required to provide children with 12 months of continuous Medicaid eligibility, and 10 states are moving ahead on longer periods of continuous coverage for children up to age 6.
These advances, however, are now at risk. When continuous coverage ended on April 1, states were permitted to resume Medicaid terminations—and the ensuing months have been disastrous for families who already struggle to make ends meet even with health insurance. At least 70% of the more than 12.5 million people disenrolled from Medicaid since April have lost coverage not because they were deemed ineligible, but for procedural reasons such as states having outdated contact information or participants not receiving renewal applications. The most recent data reveal that 3 million fewer children are enrolled in Medicaid—a very troubling statistic since the vast majority are likely still eligible.
This is a moment to invest in Medicaid, not abandon it. Policymakers must meet the moment with the urgency it requires.
First, the 10 states that have not expanded Medicaid under the ACA should do so. A recent Urban Institute report funded by the Robert Wood Johnson Foundation finds that if those states expanded Medicaid, enrollment would increase by 5 million people, nearly half of whom are currently uninsured. Researchers estimate that the overall uninsurance rate in those 10 states would drop by 25% if they all expanded, with the largest declines among Black adults. These states must act. If they continue to sit on their hands, Congress should pursue a federal solution to closing this coverage gap.
Second, all states should manage the end of continuous Medicaid coverage more responsibly. No one—especially children—should lose health care coverage over a technicality. States should take considerable care to ensure that anyone eligible for Medicaid does not get removed erroneously, and the federal government should kick in additional resources and technical assistance to help. States should also follow Kentucky and North Carolina’s lead by pausing renewals for all children for 12 months, which will streamline enrollment for kids while helping to free up time and resources to process renewals for adults.
Finally, states should help people who are no longer eligible for Medicaid find alternate health care coverage. More than 15 million people nationwide have already signed up for marketplace plans in the current enrollment period, which ends on Jan. 15. Thanks to the Inflation Reduction Act, expanded federal subsidies that can reduce or even eliminate premium costs for those plans remain in place through 2025. States should move quickly to ensure that residents suddenly caught without coverage know their options and receive new coverage as quickly as possible. And Congress should make those subsidies permanent.
For North Carolina residents like Sheila—a single mom whose daughter was born with a birth defect that has required years of care—Medicaid means everything. As Sheila put it, “Medicaid saved my kid’s life.” Millions of people throughout the United States have similar stories. Policymakers ought to listen to them.
Avenel Joseph, Ph.D., is vice president for policy at the Robert Wood Johnson Foundation (@DrAvenelJoseph).
NEXT STORY: Child care gaps in rural America threaten to undercut small communities





