As xylazine surges, some lawmakers want jail time for dealers and people who use the drug
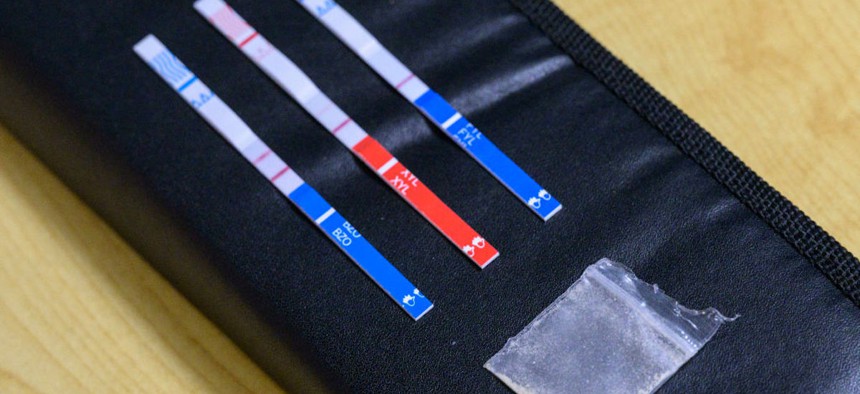
Tests strips, used to detect the presence of fentanyl and xylazine in different kinds of drugs, such as cocaine, methamphetamine, and heroin, lay next to a bag of heroin at St. Ann's Corner of Harm Reduction in New York City on May 25, 2023. ANGELA WEISS/AFP via Getty Images)

Connecting state and local government leaders
The animal sedative is cheap, easy to get and sometimes winds up in other illicit substances.
This story is republished from Stateline. Read the original article.
Legislators in a handful of states are offering bills to address the rise in the misuse of xylazine, a cheap animal sedative not intended for human consumption.
Xylazine, or “tranq,” can induce blackouts and cause lesions that sometimes result in severe infections or amputations, and it can even lead to death. The opioid overdose-reversal drug naloxone does not work on xylazine, which drug dealers often find through the dark web and other illicit channels, rather than getting it from veterinary offices. Although xylazine isn’t classified by the federal government as a controlled substance, it also isn’t approved for human use.
Several states—including Indiana, New York, South Carolina, South Dakota, Virginia and Wisconsin—are considering bills. The legislation ranges from classifying xylazine as a controlled substance to stiffening criminal penalties for possession and distribution, as well as legalizing testing strips so people who intend to take drugs can make sure they aren’t tainted by xylazine.
Other states—Florida, Ohio, Pennsylvania and West Virginia—have already added xylazine to their lists of controlled substances, which adds tighter controls to the storage and movement of the drug for veterinary use.
The accessibility and affordability of xylazine, which can be bought online from Chinese suppliers for $6 to $20 per kilogram, make it an attractive option for drug traffickers, according to the federal Drug Enforcement Administration. Xylazine is frequently used as an adulterant to enhance the psychoactive effects of other drugs, such as fentanyl. Yet many people who use such drugs don’t realize that xylazine has been mixed in.
Public health experts and harm reduction advocates, who work with people who use drugs to help them avoid the worst outcomes, warn that criminalizing xylazine or categorizing it as a controlled substance will just exacerbate the fear and stigma associated with the drug, isolating people who use it and discouraging them from seeking treatment.
“Scheduling drugs and making things illegal has never had any meaningful effect … on people actually ingesting drugs or the amount of drugs showing up in the drug supply,” said Colin Miller, the community liaison and social/clinical research specialist at the University of North Carolina Street Drug Analysis Lab. “Xylazine is just like the latest in a long line of these examples.”
Danielle German, an associate professor at the Johns Hopkins Bloomberg School of Public Health, agreed that ratcheting up penalties will do more harm than good, “even if the legislation is coming from a place of good and wanting to help.”
“That increased perception of penalty—we’ve seen over and over and over again that that’s what pushes people away from the resources that we most want them to be able to access,” German said.
State Action
Nevertheless, several states are embracing a get-tough approach.
In South Dakota, Republican Gov. Kristi Noem in February signed legislation classifying xylazine as a controlled substance, with fines and penalties of up to two years in prison for using, manufacturing and distributing the drug, while still allowing for veterinary use.
A similar bill is pending in South Carolina, where manufacturing or distributing the drug for other than veterinary use would bring a felony charge and up to 10 years imprisonment. Virginia lawmakers are considering legislation with similar penalties.
In New York state, legislation would place xylazine in the category of the most dangerous controlled substances, which would carry stiffer criminal penalties for both possession and distribution.
In Indiana, a bill making its way through the legislature would criminalize the possession and distribution of xylazine, with potential punishment of jail time. It would add steeper penalties for repeat offenders. The bill exempts use and distribution for veterinary purposes.
“I fully support other harm reduction avenues, such as [the opioid overdose-reversal drug] Narcan and test strips,” said Indiana Republican state Rep. Jennifer Meltzer, the bill’s author. “I just believe that we also need to go after the bad actors. … Having a criminal effect will hopefully deter individuals that are dealing or maybe even individuals who are now only seeking out xylazine, to get the help that they need.”
Another bill in Indiana would have legalized testing strips for all controlled substances, including xylazine, but it died in the Senate. Meltzer, one of the bill’s co-authors, plans to work with the Democratic lead author of that bill to get it passed during the next legislative session.
But in Wisconsin, legislation to legalize xylazine testing strips is awaiting the governor’s signature.
Xylazine’s Spread
Xylazine was first detected in other drugs in Puerto Rico in the early 2000s, according to the DEA. Now, the drug can be found across the states, though available research suggests that xylazine-involved overdose deaths are primarily concentrated in the eastern United States, especially in the Northeast.
The University of North Carolina Street Drug Analysis Lab tests drug samples sent by over 150 harm reduction and syringe exchange programs across 35 states and publishes those results publicly. Between January 2021 and February 2024, the lab found xylazine in lab-confirmed fentanyl samples from 15 states. Some of the samples analyzed were submitted to the lab because people suspected the presence of xylazine, Miller wrote in an email to Stateline.
The states with the highest number of fentanyl samples that tested positive for xylazine are North Carolina, 148; New York, 148; Michigan, 66; Pennsylvania, 38; and Washington, 20.
You can’t say that you want people to stop using drugs and then every time I call for a detox bed, there’s not a bed.
– Alixe Dittmore, housing and shelter capacity building coordinator with the National Harm Reduction Coalition
But some harm reduction advocates and public health experts argue that focusing too heavily on xylazine could inadvertently facilitate the entry of other, potentially stronger and more harmful drugs into the illicit drug supply. They warn that what states are doing now to curb xylazine use repeats a strategy that has had limited success with substances such as fentanyl.
“Because we hyper-focused on fentanyl for so long, the criminal drug market responded with a more lethal and potent substance to adulterate and then dominate the supply,” said Sarah Laurel, the founder and executive director of Savage Sisters Recovery, a Philadelphia nonprofit that offers free services to people experiencing homelessness and substance use.
Philadelphia is one of the cities that has been hit hardest by the surge in xylazine use. In 2022, the Philadelphia Department of Public Health found that xylazine was involved in 480, or more than a third, of the 1,413 unintentional overdose deaths. Almost every death in which xylazine was found also involved fentanyl, according to the agency.
“The same thing will happen if we have a new focus on xylazine. They are just going to find a new substance that is going to satisfy the demand,” Laurel said.
Instead, some advocates say states should focus more on expanding access to substance use treatment services and mobile drug-checking equipment, such as mass spectrometers that can analyze ingredients within a drug mixture.
“You can’t say that you want people to stop using drugs and then every time I call for a detox bed, there’s not a bed,” said Alixe Dittmore, the housing and shelter capacity building coordinator with the National Harm Reduction Coalition.
“We have incredibly punitive and prohibitive services,” Dittmore said. “You really have to holistically look at it when you’re worried about how many folks are passing away.”

NEXT STORY: Lawmakers across the U.S. seek to curb utility spending on politics, ads and more extras




